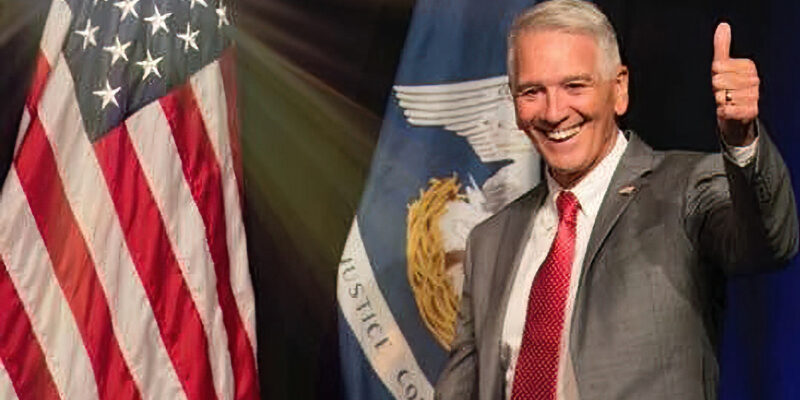
Incoming governor Republican Atty. Gen. Jeff Landry, for now, is showing he’s seeking a home run when it comes to smaller, more efficient – and more effective – government. As part of his introduction of new (and solid) appointees to his administration, he noted willingness to establish co-payments and work requirements for Medicaid recipients in Louisiana.
Medicaid blows away any other single spending item in the state’s budget. The latest projections have it spending $3.75 billion this year in state taxpayer dollars, which in terms of those dollars only elementary and secondary education rivals, but throwing in $13.5 billion in federal dollars means about three-eighths of total state spending goes out the door for this program.
Cost sharing and community engagement requirements of some program recipients not only could return a little offsetting revenue but also could result in wiser utilization that reduces costs. Clients, properly incentivized, tend to behave more responsibly in their consumption of health care on the dole. Research profusely demonstrates over a variety of welfare programs that asking for exchanges of resources with clients, whether that be cash, labor, or action or desire to participate in the paid or unpaid workforce, reduces dependency on welfare without a decline in well-being of the clients.
However, the legal environment and the nature of health care as a relative demand-inflexible good make creation of incentive programs like these a little tricky. Cost-sharing for Medicaid is allowed under federal law, but exempts a significant minority of clients, and at low permissible rates unchanged for a decade. Further, as expected when people are asked to pay more for a good, cost-sharing leads to lower utilization of Medicaid, which potentially could lead to those with the least resources less able to access health care.
While that cudgel often is used by leftist special interests to argue against any form of cost sharing, which fewer than half the states employ, in fact the latest research reveals that of those who drop out of Medicaid with the introduction of cost sharing typically are the healthiest who don’t need it (and if they find they do, they typically re-enroll).
In other words, cost sharing (at ridiculously low maximum levels such as $75 for hospitalization, $4 for a doctor visit and $8 for nonemergency emergency room use, with a cap of five percent of income) doesn’t really discourage clients who need Medicaid.
Louisiana charges only low copayments on prescription medicine, $0.50 to $3. It doesn’t charge what it could for anything else or on managed care premiums, but if it did, older data suggest it could save $175 million annually. And that doesn’t include savings from more efficient use of resources caused by cost-sharing; such savings certainly exist but no study has been able to quantify them for any jurisdiction.
Community engagement is more complicated. For one thing, the legal environment as shaped by present jurisprudence makes it difficult for states like Louisiana who unwisely expanded Medicaid to impose this, as lower federal courts through 2020 ruled that imposing such a requirement, even upon as was the case just able-bodied adults without dependents years prior to retirement age (ABAWDs), in a strict legal sense didn’t comport to the law establishing Medicaid that mandates any waiver to its requirements not reduce the prospects of the client population.
That could change with the current U.S. Supreme Court lineup that might take a more holistic approach to this question and rule in favor of introducing community engagement. That may come. After several states tried this and were found wanting in the courts, and further found the Biden Administration hostile to these efforts, most of those states abandoned such efforts. But a few states are gearing up to try again and take the Biden Administration all the way to the Supreme Court if necessary, if not wait for a more flexible future administration to aid them.
Advertisement
Absent that, the only such program now in existence is Georgia’s, because its work/volunteer/student requirement program for ABAWDs is for anyone in the expanded zone, which Georgia wisely has yet to accept. And it had to fight the Biden Administration in court to get it underway, which finally happened earlier this year, in showing raw numbers of Medicaid-insured would go up.
However, because it hasn’t expanded Medicaid, it has decided to pay entirely for some insurance benefits for qualifying clients, which is less than it would pay under expansion but with potentially many fewer recipients. But, the point of the program isn’t so much as to insure the uninsured but to let them use the program as a bridge to obtaining insurance through the private sector through employment that offers that as a benefit.
Another issue with requirements for the Medicaid population is, because of federal law that makes it so easy to receive care without paying by citing indigency, strictures often can be dodged easily while still receiving care. This is why such requirements have but a negligible effect on promoting work when applying those to other welfare programs can produce dramatic changes. That’s why a community engagement requirement that the Republican-led U.S. House of Representatives had on the table earlier this year would have knocked out only an estimated 52,700 (expansion) clients in Louisiana at a total of $34.5 million in state costs.
So, what Louisiana could do is abandon the Medicaid expansion and use the Georgia model. That would provide an instant $451 million in savings, some of which then would be plowed back into the 25 to 100 percent federal poverty limit clientele for stripped-down insurance, with about a third to a half in the past already able to pay for their insurance likely through the workplace, so the uninsured portion won’t rise much and the state will pay less for insuring those who really need it and will give back to the community in some form.
Excitingly, with these reforms Landry is swinging for the fences that could result in a huge payoff by trimming state government to the tune of several hundred million dollars while the deserving poor obtain health insurance and care when they feel they need it. It’s been years since health care policy in the state could find itself on such a healthy trajectory.
Advertisement
Advertisement